The business case for embracing electronic prior authorization, or ePA, nationwide seems overwhelming. Current prior authorization processes are a chief driver of provider and patient frustration. Needed investment in FHIR APIs is now mandated by CMS Rule 0057, and ePA pilots report dramatic efficiency gains. More specifically, providers in such pilots were automatically notified that no prior authorization was needed for 50%-85% of requests. Nonetheless, reservations about the scalability of ePA persist and, in turn, spur questions about the minimum investment needed just to comply with CMS 0057.
Insights from Leader Roundtables
To better understand these contrasting viewpoints, InterSystems conducted a series of roundtables where a cross-section of leaders each identified up to three top-barriers to scaling ePA from point-to-point pilots to a national norm for processing prior authorization requests. In total, 45 health plan leaders made 132 selections from a picklist of 19 possible roadblocks. The results indicate that scaling ePA is by no means just a technology challenge. While “siloed systems” was the most common top barrier, “aversion to changing workflows” placed a close second. It was also the top-rated barrier among the roughly 50% of roundtable participants overseeing IT and interoperability, as opposed to those leading clinical and administrative operations.
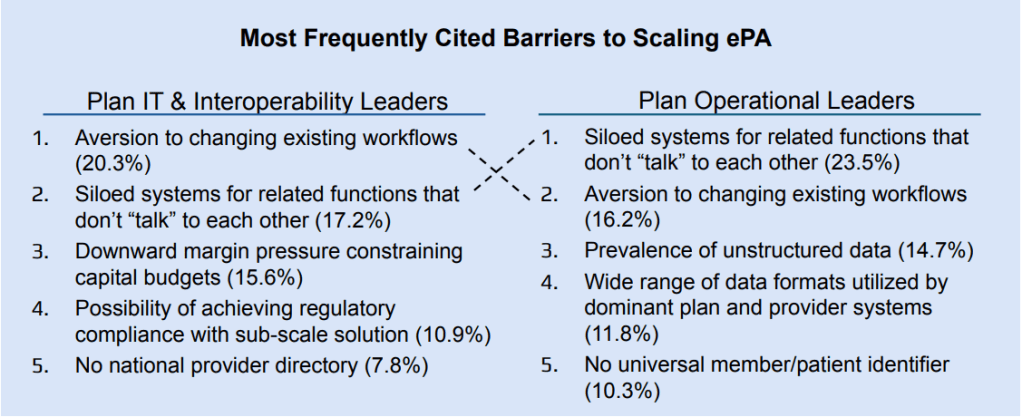
In addition, barriers named by these two groups diverged altogether after the top two. IT and interoperability leaders focused next on budget pressures, whereas operational leaders raised questions about available data. Capital constraints and alternatives for achieving regulatory compliance with subscale solutions together account for 27% of barriers prioritized by IT and interoperability leaders, compared to just 7% by operational leaders. In contrast, the prevalence of unstructured data and wide range of data formats account for 27% of barriers prioritized by operational leaders, compared to just 8% by IT and interoperability leaders.
Best Practice Recommendations
Leading organizations working with InterSystems are employing a bundle of tactics to overcome these disconnects among stakeholders who must collaborate to scale ePA. These include:
- Expanded process mapping—Recognizing that people are more likely to embrace workflow changes that address common frustraters, leading plans are expanding process-mapping efforts to pinpoint staff most likely to be impacted by ePA adoption and time-consuming workarounds for shortfalls in current prior authorization processes that ePA can address.
- Staged roll-out— Many of the provisions in CMS 0057 are strongly recommended rather than required, allowing plans to weigh organizational readiness and their larger strategy for scaling ePA when setting timelines for rolling out recommended changes, such as digitization of medical rules and real-time responses to prior authorization queries.
- Upgrades key to unlocking data liquidity—With prior authorization workflows typically involving a wide range of legacy systems, leading plans first ensure their stacks include an API manager and data integration engine capable of routing queries to the right existing system and normalizing disparate data streams.
Lastly, ePA champions must quantify efficiency gains beyond the number of services for which no prior authorization was required to win broad provider buy-in. While not one health plan participating in our roundtables identified “insufficient evidence of quantifiable, concrete ROI” as a top barrier, it ranked third among our 14 provider participants.

For more information, Listen to the InterSystems webinar hosted by Becker’s on Roadblocks to Scaling Electronic Prior Authorization and How Leaders Are Moving Forward and view our solutions at InterSystems Payer Services.
